Do frequent digestive problems like bloating, diarrhea, and abdominal pain affect your daily life? You’re not alone.
Gastrointestinal troubles can result from a number of health conditions. But for approximately 7% of the U.S. population, gluten – a protein found naturally in wheat, barley, and rye – is a contributing factor to digestive issues.
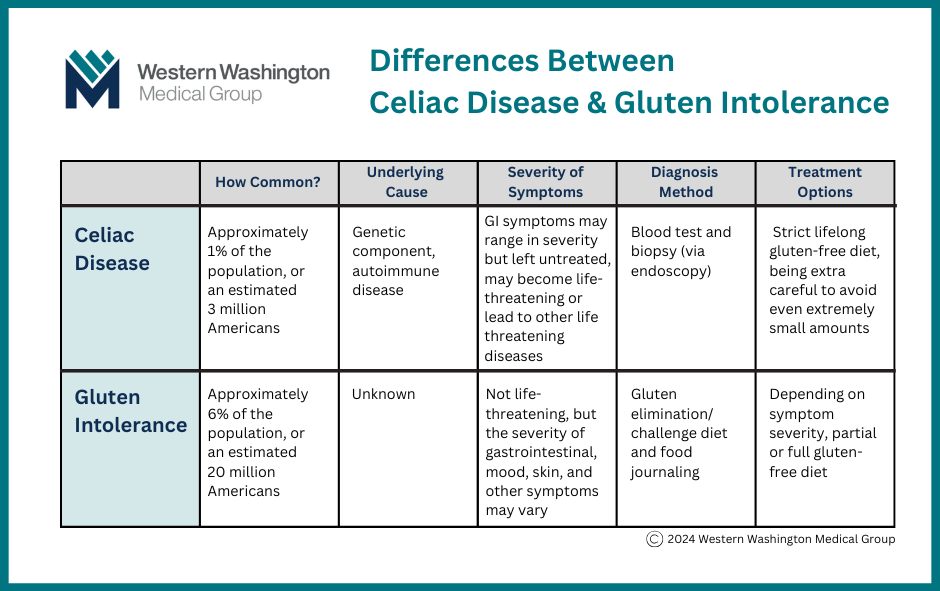
While the terms “celiac disease” and “gluten intolerance” are often used interchangeably, these are two different conditions that have different effects on your health.
Let’s clarify the differences and explore how patients can manage these uncomfortable conditions.
What is Celiac Disease?
Celiac disease is a serious autoimmune condition characterized by stomach pain and chronic digestive problems.
Celiac causes the body’s own immune system to damage the villi (small finger-like structures) that line the small intestines. Villi perform an important role in digestion by absorbing nutrients and minerals from the food we eat. When villi are no longer able to do their job, malabsorption – which can lead to malnutrition – and digestive problems can occur.
Roughly 1% of the population has celiac disease. For individuals with celiac, flare ups are triggered when they eat foods with gluten in them.
Symptoms of Celiac Disease
Symptoms of celiac disease can include:
- Fatigue that interferes with daily activities
- Stomach aches or abdominal pain
- Diarrhea or constipation
- Bloating and/or gas
- Decreased appetite
- Nausea or vomiting
- Weight loss
- An itchy, blistering rash
While those symptoms are unpleasant enough, people with celiac disease are at greater risk for developing small bowel cancers and coronary artery disease.
In addition, patients who don’t get treatment for celiac disease may develop other autoimmune conditions such as type 1 diabetes, thyroid or endocrine disorders.
Who is at Risk for Celiac Disease?
Doctors don’t fully understand what causes celiac disease, but like most autoimmune conditions, there is a genetic component. Individuals are more likely to develop celiac if they:
- Have a family member with celiac disease
- Were assigned female at birth
- Are White
- Have another autoimmune disease, such as rheumatoid arthritis
- Have a chromosomal disorder, such as Down syndrome
How is Celiac Disease Diagnosed?
There are two methods providers use to diagnose celiac disease: a blood test and a biopsy. Often, these two tests are used together. Your primary care provider may order the blood test and then refer you to a gastroenterologist for the biopsy and further evaluation.
Once the patient consults with a GI doctor and a biopsy is recommended, an upper endoscopy procedure is then scheduled.
During the upper endoscopy, the patient is put under sedation. A small camera on the end of a long, flexible tube is passed down their throat so the doctor can look at the small intestines and take a sample of the tissue (biopsy) for further analysis.
If it’s confirmed that the patient has celiac disease, the provider may order another blood test to check for nutritional deficiencies.
Treatment for Celiac Disease
There is no cure for celiac disease, but it can be treated. The treatment is simple, but (for many) is not easy: absolute avoidance of any food containing gluten.
Gluten is often hidden in foods you wouldn’t expect, so it’s important to read every food or drink label before consuming it. Even tiny amounts of gluten in foods like a breadcrumb, a dusting of wheat flour, or a splash of soy sauce can cause damage to the small intestines.
Fortunately, there are many gluten-free foods available today that taste good and are easy to find, especially in the Pacific Northwest.
=====
What is Gluten Intolerance?
Gluten intolerance is a sensitivity to gluten. Some people are born with this sensitivity, others develop it later in life.
Unlike celiac disease, gluten intolerance is not an autoimmune condition and it does not have a genetic component. It is also not a wheat allergy (which is characterized by hives, stuffy or runny nose, sneezing, headaches, asthma, or anaphylaxis.)
It is estimated that approximately 6% of the population are gluten intolerant. The condition is more common than celiac, and more common in people assigned female at birth.
What Are the Symptoms of Gluten Intolerance?
Many symptoms of gluten intolerance are similar to those of celiac disease, including:
- fatigue
- abdominal pain
- diarrhea or constipation
- bloating or gas
- nausea or vomiting
- depression
- anxiety
- brain fog
- headache
- joint pain
- skin rash
How is Gluten Intolerance Diagnosed?
If, after reviewing your medical history and current symptoms, your primary care provider suspects you have gluten intolerance, they will first order lab tests to rule out celiac disease or a wheat allergy.
If your bloodwork indicates that you have celiac disease, your primary care provider will refer you to a gastroenterologist for further evaluation and treatment. If you have a wheat allergy, your provider may refer you to an allergist.
If your lab tests show that you don’t have celiac or a wheat allergy, your healthcare provider will ask you to do a subtraction diet. This means, avoid all foods with gluten and keep a food journal where you note what you ate, when you ate, and what symptoms you experienced – if any – for a period of six weeks.
If your symptoms improve, you will be asked to slowly reintroduce gluten back into your diet. If the symptoms return, it’s most likely because you have a gluten intolerance.
Treatment for Gluten Intolerance
Like celiac disease, there is no cure for gluten intolerance. However, since a gluten intolerance doesn’t have the same potentially life-threatening complications as celiac disease, your provider may recommend you follow a partial or completely gluten-free diet (depending on the severity of your symptoms).
=====
=====
Treatment Options: Living Gluten-Free
For patients with celiac disease or gluten intolerance, making changes and sticking to a gluten-free diet can be a challenge. Many of your favorite foods may now be off limits, but there are likely to be similar gluten-free versions that are still satisfying.
Here are some tips for living a gluten-free lifestyle:
Read all labels, all of the time
As manufacturing processes and ingredients can change, products that were gluten free in the past may now have gluten-containing ingredients. Read the ingredients list on product labels and look for anything that mentions wheat, barley, or rye.
Also look up any additives you are not familiar with. Often times, they aren’t gluten-free. Many brands now list their package ingredients online, so a simple web search can help you choose what to buy.
Look for gluten-free foods at the grocery store or online
Most grocery stores have a gluten-free section, or clearly tag gluten-free items on the shelf to make them easy to find.
Online grocery shopping websites usually enable you to search for gluten-free foods, although you will still want to double check the labels and verify ingredients before you buy.
How to order at restaurants
If you eat out, it’s best to look through the menu in advance. Thankfully, many restaurants now have their menus listed on their websites. Some may even include a link to nutrition and allergen information where you can identify which menu items are safe for you to eat.
Some restaurants will have a dedicated gluten-free menu, others may have symbols on the menu that indicate gluten-free or gluten-friendly.
If you can’t check the menu in advance, call ahead or ask your server about what gluten-free options they offer. If they don’t know which items are gluten free, or don’t know how to alter their menu to be safely gluten-free, you probably shouldn’t eat there.
Conclusion
Understanding the difference between celiac disease and gluten intolerance is crucial for managing digestive symptoms and improving one’s overall health. If you suspect you may have either condition, request an appointment with a WWMG primary care provider for proper diagnosis and treatment.
By working closely with your provider and making any necessary dietary changes, it’s possible to effectively manage your condition so you can enjoy a better quality of life.
For more information on celiac disease and eating gluten-free, visit celiac.com.