A pacemaker keeps your heart beating with a normal rhythm, but not always pumping as efficiently as it should. In recent years, a new method of implanting pacemakers has allowed the heart to utilize its natural electrical pathway to function more efficiently. This is called cardiac physiological pacing (CPP) or conduction pacing.
Read on to learn more about CPP and how this technological advancement works to help patients improve their heart function and reduce the chance of hospitalization.
Your Electric Heart
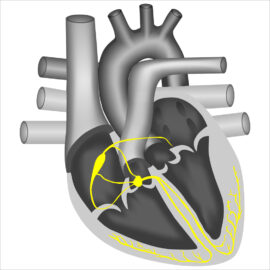
The conduction pathway of the heart can be likened to an electrical circuit in which the electrical current travels through tissue instead of wires.
The heart’s electrical activity goes from north to south and from the center out. That is the most efficient and effective way for the heart to be pumping our blood out to the vital organs.
In a healthy heart, that electrical pulse travels through the conduction pathway at a regular resting pace that ranges from around 60 to 100 beats per minute.
When a patient’s heart beats too slowly, or has irregular pauses, their Cardiologist may recommend a pacemaker. Pacemakers are usually prescribed for individuals that have a slow, abnormal heart rhythm or symptoms related to a slow heart rate.
Traditional Pacemakers
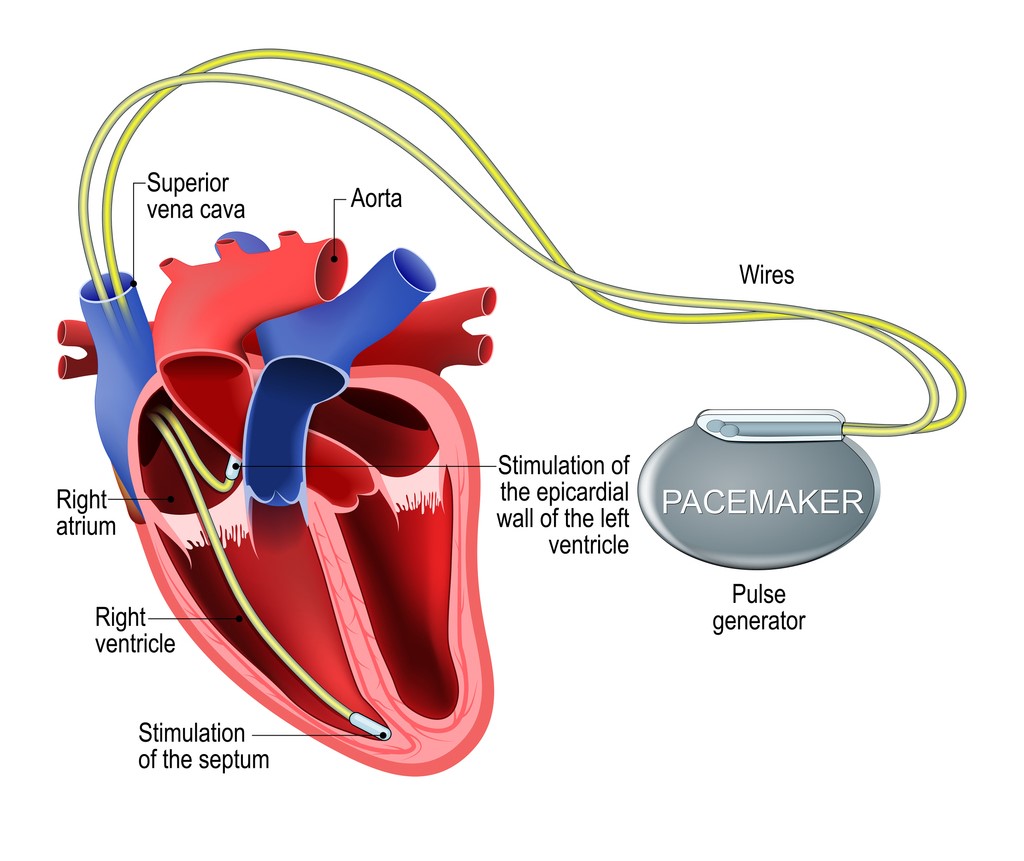
Typically, a pacemaker connects to the heart with two wires, or leads. One lead is implanted in the right atrial appendage, which is a small pouch in the upper chamber of the heart.
The other lead gets implanted into the right ventricular apex, at the tip of the lower chamber of the heart. This ensures correct pacing of the heartbeat, but it does not replicate the natural circuit of electrical activity that stimulates the heartbeat.
A traditional pacemaker sends electricity upwards and right to left, rather than the natural directions of downwards and from the center out.
Cardiac Physiological Pacing
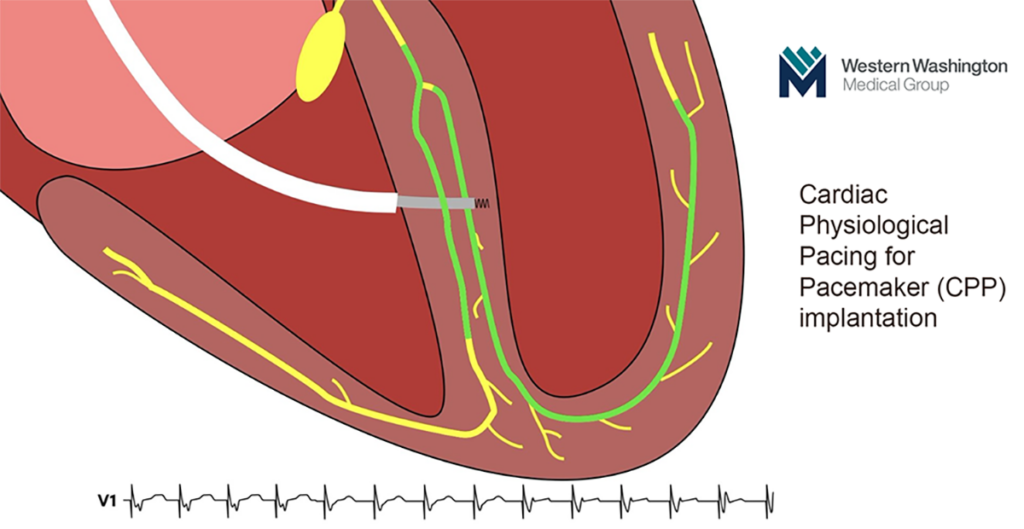
Physiologic pacing requires placing the wires differently in order to engage the natural conduction system of the heart.
The pacemaker wire is embedded into the specialized tracks that allow for quick electrical activity. It enables the natural ability of the heart to squeeze and pump out blood to the vital organs. Doctors have known since the 1960s that a pacemaker that could replicate not only the pace but also the pathway of a healthy heartbeat would be preferable. But until recently, it was not possible.
A Cardiac Electrophysiologist explains, “It’s a very technical procedure, with very small targets to aim for in the heart. For us to engage those particular areas we have to maneuver the wires in a more specialized way than how we learned to do a traditional pacemaker 10-15 years ago.”
Compared to the traditional wire placement that has a margin of error within a centimeter or more, attaching pacemaker wires to the heart’s specialized conductive tissues has a margin of error measured in millimeters. That level of accuracy requires advanced tools and imaging that were not available until 2015.
CPP Implantation
The techniques for implanting pacemakers with physiological pacing are not performed by a general Cardiologist or even among heart rhythm specialists. Only a few specially trained Cardiac Electrophysiologists have the advanced training to perform the newer procedure.
Western Washington Medical Group’s Dr. Garhwal was an early adopter of CPP and is now among the most experienced and skilled CPP surgeons in the Puget Sound region.
From the patient’s perspective, getting a CPP pacemaker implanted is no different from the traditional pacemaker surgery, performed as an outpatient procedure at a hospital. During surgery, the pacemaker and the wires are inserted through a 2-inch-wide incision near the left collarbone, and the wires are placed using MRI and live X-ray guidance.
After surgery, patients should avoid strenuous activity for about a month, but don’t need to remain entirely inactive during the recovery period. In order to avoid getting frozen shoulder, patients can move their left arm freely, while keeping the left elbow below the shoulder for four weeks.
Most patients are able to manage post-operative pain simply with Tylenol or ibuprofen.
Risks of CPP Surgery
Every surgery comes with some risk, including the risk of infection, and when the heart is involved, some of those risks are serious.
A Cardiac Electrophysiologist explains, “The scary stuff like heart attack, stroke or death is extremely rare, almost negligible. It’s less than 0.1%… The risks from a conduction system pacemaker are no different from the risks of a traditional pacemaker, with one caveat. Since a conduction system pacemaker is getting implanted in a very particular area of the heart, there have been some case reports of injury.”
Small arteries or nearby tissue can be damaged, and perforation from the right lower to the left lower chamber is possible. Typically, these injuries do not require intervention, but can result in increased pain during the recovery period.
The heart has an amazing ability to adapt, and in most patients, the heart muscle seals off any damage on its own. Like more serious risks, tissue damage is extremely rare. Adverse incidents are declining as imaging technology improves and surgeons gain increased experience with the CPP technique.
Benefits of CPP Implantation
In contrast to the rarity of negative outcomes, the benefits of physiologic pacemakers are significant, even compared to a traditional pacemaker.
For patients that are at risk of heart failure, having a traditional pacemaker will put them even more at risk for worsening heart failure and even hospital admissions. Whereas if they get a conduction system pacemaker, the heart will not know the difference in terms of the way that it’s electrically being activated, yet it will still remain as efficient as possible.
Studies show that patients who have pacing-induced cardiomyopathy and get upgraded to a physiologic pacer are more likely to improve their heart function and stay out of the hospital compared to those that don’t.
Do You Need CPP?
For anyone with a pacemaker whose current condition is satisfactory, our Cardiologists do not recommend upgrading to a new device. Upgrading an existing pacemaker is only recommend for three types of patients:
- Patients who have evidence of declining heart function
- Patients with worsening heart failure, for example, resulting in repeat hospitalization during a year
- Patients whose heart function hasn’t improved despite best efforts with medications and cardiac resynchronization therapy
For new patients who need a pacemaker, physiological pacing is a superior option. The first step is to reach out to a cardiologist.
If you don’t have a cardiologist, especially if you already have a pacemaker, request an appointment WWMG Cardiology. Anyone with a pacemaker needs to be monitored by a cardiology team.
All of our cardiologists are aware of the benefits of conduction system pacing and are a little more aggressive about asking for it when it is indicated. WWMG Cardiologist Ravi Mahidhar agrees. “I think that’s a great option for patients who need a permanent pacemaker to maintain the normal physiological connection system, and I strongly recommend it for my patients who need a permanent pacemaker,” he said.
Although few cardiologists can perform physiologic pacing implant surgery, they can make the referral to WWMG Cardiac Electrophysiologist Dr. Sanjeev Garhwal.
If you’re a heart patient in need of a pacemaker, or already have one and your health is declining, contact WWMG’s Cardiology team to discuss if cardiac physiological pacing is right for you. Our Cardiologists are here to help.