It’s natural to be nervous about any invasive procedure involving your heart, but understanding what’s involved can help you get through it with confidence. If you have coronary artery disease (atherosclerosis) your cardiologist may recommend an angioplasty with a stent placement to treat it.
Atherosclerosis – the most common type of heart disease – is caused by a buildup of cholesterol plaque in the coronary arteries. That buildup narrows the heart’s arteries and eventually blocks blood flow, which can lead to heart attack, stroke, or other life-threatening conditions.
Angioplasty is a procedure that opens blood vessels when they are narrow or blocked. To treat atherosclerosis, angioplasty with a stent placement can restore blood flow to the heart by clearing the cholesterol plaque from a coronary artery.
Who Should Get a Coronary Stent
Stent placement via angioplasty is for patients who have cholesterol plaque blockages in their coronary arteries.
The most common event that precedes a stent placement is a heart attack. However, cholesterol plaque blockages are also discovered when patients experience symptoms such as:
- chest pain
- abnormalities on stress tests, or
- heart rhythm problems.
Dr. Vinaya Chepuri, a Western Washington Medical Group Cardiologist, explains, “All of those are clues that you might have blockages or cholesterol plaque buildup in your coronary arteries. Those are the patients that do well with stent placement. It’s a same-day [outpatient] procedure unless it’s happening in the setting of a heart attack.”
“When people experience a heart attack, it’s been proven over and over that those patients are best treated by finding the location of the blockage with an angiogram and opening [up the blood vessel] with a stent. We take them to the cath lab immediately to open up the blocked or narrowed coronary artery and restore blood flow,” said Chepuri.
The Process of Stent Placement
A plumber clearing a clogged pipe with a drain snake is a crude but appropriate analogy for angioplasty. Whether done as an inpatient or outpatient procedure, an angioplasty for stent placement is performed in a hospital. Patients are sedated during the procedure but are not unconscious.
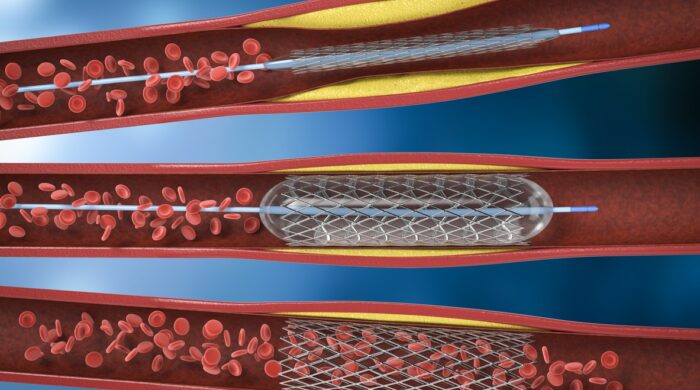
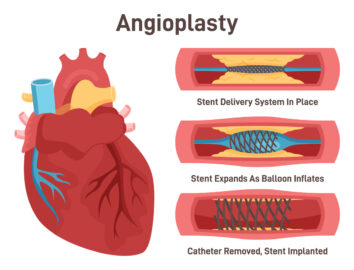
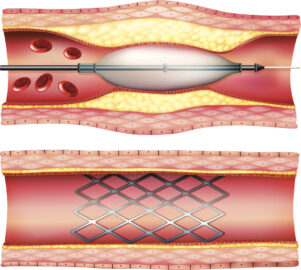
During the angioplasty, an interventional cardiologist inserts a tiny tube (a 2mm catheter) into an artery, usually at the patient’s wrist, which is threaded up to the heart. A stent is mounted on a balloon that travels through the catheter to the blockage, which has been made visible on X-rays using an injected dye.
At the blockage site, the balloon with a stent mounted on it is expanded, thus pushing it up against the wall of the artery to open the blood vessel. Then the doctor deflates and removes the balloon and the catheter, leaving the stent behind to support the artery walls.
The stent acts as a sort of buttress to prevent the artery from collapsing. Most stents are also coated with slow-release drugs that help to prevent the excessive buildup of scar tissue during the recovery period.
After an outpatient procedure, patients spend 4-6 hours in recovery and can usually go home the same day. To protect the catheter insertion point, patients should not lift anything heavy for a few days but can usually return to full activity within a week.
Patients recovering from a heart attack will need to stay in the hospital longer.
What is a Coronary Stent?
“The stent is like a wire mesh tube that keeps the artery open,” explains Chepuri. “It stays there permanently, and because it’s a foreign object, your body is going to want to clot it off.
“So you have to be on blood thinners for six months to a full year until the stent fully heals up. After that time, we know that scar tissue covers up the metal and we can take people off some of the blood thinners.”
The Most Important Part of Recovery
Although recovery from the angioplasty procedure is quick, healing continues inside the heart for months or up to one year. The most important part of long-term recovery – and the biggest risk after an angioplasty – comes from the patient’s behavior post-surgery.
Chepuri emphasizes it’s important for patients to “Make sure they are taking their blood thinners without fail, especially in the first couple of weeks. We’ve had patients get blood clots on the stents that cause a heart attack when they’ve missed even one or two doses of their blood thinners. Taking the blood thinners for a full year is really important” for a positive recovery.
Risks of Stent Placement
However, as with any invasive procedure, there are some immediate risks, which can include major complications such as a stroke, heart attack, or death.
“The risk varies depending on how urgently you need the procedure. The risk of a major complication for a person who is having this procedure done electively is less than 1%. But for a person in the midst of a heart attack, the risk of stroke or cardiac arrest goes up to 3-5% because their heart is already under stress. The risk is still not that high compared to the benefits,” said Chepuri.
This is true even when heart attack patients have dangerous complications, because restoring blood flow during a heart attack has much better outcomes for the patient than doing nothing. “In some cases, the risk of dying is virtually 100% if they do nothing,” said Chepuri. But he would much rather keep the risk low with earlier intervention.
Preventing Future Artery Blockages
Angioplasty with stent placement restores blood flow immediately and significantly.
“But a stent doesn’t prevent future blockages. Risk factor modification is still important,” warns Chepuri.
While you can’t do anything about the #1 risk factor for atherosclerosis – your family history – patients with stents can control or manage other important risk factors by:
- quitting smoking
- managing their diabetes
- establishing a healthy diet, and
- exercising regularly.
“Even if they have normal level cholesterol, we recommend cholesterol medications,” said Chepuri. Whatever the patient’s previous cholesterol level was, that patient had coronary cholesterol plaque buildup, indicating the need to lower their cholesterol.
“It’s one of the hardest things to get a patient to recognize, but statins have been proven to reduce cholesterol cholesterol plaque buildup and reduce heart attacks and other cardiac events.”
What to Do If You Have Symptoms
It’s important to seek medical advice at the first sign of trouble, because the severity of a heart condition raises the risk of having a procedure to treat it,.
“Do not ignore your symptoms. Get medical attention sooner rather than later,” said Chepuri.
“The earlier they come in to have things evaluated the less risky the procedures are if they need them. I see a lot of patients who come in with chest pains and they never end up needing an angiogram or stent because we can take care of things with medication, diet and exercise.”
Seeking treatment earlier may enable you to prevent the need for invasive treatment later. If you have one or more of the risk factors associated with heart disease and are concerned, make an appointment with your WWMG Primary Care provider. They can advise on lifestyle modifications, medication, or refer you to a Cardiologist.
If you’ve already been diagnosed with heart disease, or are at high risk of a cardiac event, contact WWMG Cardiology for a thorough assessment. Our experienced and caring Cardiology team will work with you to create an individualized treatment plan to help you stay healthy for many years to come.